Views: 0 Author: Site Editor Publish Time: 2025-08-14 Origin: Site

Radiotherapy for prostate cancer lasts from 5 days to 9 weeks, depending on the treatment type chosen.
Most patients attend about 20 to 40 sessions, with each session lasting 10 to 60 minutes.
Shorter schedules like SBRT offer treatment in as few as 5 sessions, making therapy quicker and more convenient.
Doctors choose treatment plans based on cancer stage, patient health, and personal needs to balance effectiveness and comfort.
External beam radiation is the most common type, while brachytherapy and SBRT provide focused and shorter options.
Patients usually continue daily activities during treatment but may experience fatigue and side effects like urinary or bowel changes.
Clear communication with the medical team helps manage side effects and keeps treatment on track, even if schedules change.
Support services and preparation guides improve patient confidence and help them cope with the treatment process.

Radiotherapy for prostate cancer follows several common schedules. Doctors select the best option based on the patient's needs and the type of cancer. The most traditional approach uses conventional radiation therapy. This method involves about 39 to 40 sessions. Patients visit the clinic five days a week for nearly eight weeks. Each session delivers a precise dose of radiation to the prostate. The goal is to target cancer cells while protecting healthy tissue.
Hypofractionated radiation therapy offers a shorter treatment schedule. Patients receive about 20 sessions over four weeks. This approach uses higher doses of radiation per session. Many men find this schedule easier to manage. It reduces the total number of visits and shortens the overall treatment time.
Stereotactic body radiotherapy (SBRT) provides another option. SBRT uses advanced technology to deliver high doses of radiation in just five sessions. The entire treatment lasts about a week and a half. Clinical studies show SBRT works as well as longer schedules for controlling prostate cancer. Side effects usually improve over time. SBRT also offers greater convenience and may lower costs because of fewer treatment days.
Note: The main difference among these schedules is the total duration. Conventional therapy lasts about eight weeks, hypofractionation takes four weeks, and SBRT finishes in less than two weeks.
Short-course radiation has become more popular for prostate cancer. SBRT stands out as the leading short-course therapy. Doctors use precise targeting to deliver higher doses of radiation in fewer sessions. This method treats the prostate quickly and effectively. Many patients prefer short-course options because they spend less time at the clinic. The shorter treatment schedule helps men return to daily life sooner.
Short-course radiation therapy suits men with early-stage prostate cancer. It also benefits those who want to minimize disruption to work or family life. Doctors review each case to decide if short-course therapy is safe and effective. SBRT and other short schedules show strong results in clinical trials.
The length of each radiotherapy session depends on the type of treatment. Most sessions last between 10 and 60 minutes. Conventional radiation therapy usually takes about 15 minutes per visit. Hypofractionated schedules may require slightly longer sessions. SBRT sessions often last up to an hour because of the need for precise positioning and careful planning.
During each session, the patient lies still while the machine delivers radiation to the prostate. The number of sessions varies based on the treatment schedule. Doctors explain the process and answer questions before therapy begins. The medical team works to keep patients comfortable and safe throughout each session.
Tip: Patients should ask about the number of sessions and session length when discussing their treatment plan. Understanding the schedule helps reduce anxiety and prepares men for what to expect.
Doctors consider the stage of prostate cancer before recommending a treatment option. Early-stage prostate cancer often stays within the prostate gland. In these cases, radiotherapy can target the cancer cells directly and limit damage to healthy tissue. Advanced stages may show cancer spreading beyond the prostate. When this happens, doctors may combine radiotherapy with other treatments to improve results. The stage helps guide the length and intensity of the treatment plan. Patients with localized cancer usually need fewer sessions. Those with more advanced cancer may require longer or combined therapies for effective prostate cancer treatment.
A patient’s overall health and age play a major role in planning prostate cancer treatment. Doctors use special tools to assess frailty and cognitive status in older adults. For example, the G8 and Mini-COGTM tests help identify patients who may need extra support. Life expectancy is another important factor. Tools like ePrognosis, Schonberg, and Lee indexes estimate how long a person might live based on health and comorbidities. Doctors classify patients as healthy, vulnerable, or frail. Healthy patients often tolerate standard radiotherapy well. Vulnerable or frail patients may need a comprehensive geriatric assessment before starting treatment.
Note: Doctors base decisions on biological age and overall health, not just chronological age. They repeat evaluations over time to adjust the plan as health changes.
Radiotherapy can control prostate cancer in older patients as effectively as in younger ones when doctors use the right dose and technique. However, routine radiotherapy is not recommended for low-risk patients because of possible late complications. For those with heart disease, combining androgen deprivation therapy with radiotherapy may increase risks. Doctors often recommend short-term hormone therapy with radiotherapy for medium-risk patients.
Doctors create a personalized plan for each patient with prostate cancer. They review the stage, health status, and personal preferences. The plan may include radiotherapy alone or in combination with other treatments. Doctors follow guidelines from organizations like the American Society of Clinical Oncology and the International Society for Geriatric Oncology. These guidelines suggest using frailty screening and comprehensive assessments to optimize care. The doctor’s plan aims to balance cancer control with quality of life. Regular check-ins allow the team to adjust the treatment if the patient’s health changes.
Tip: Patients should ask questions and share concerns with their medical team. Open communication helps ensure the best possible outcome from any treatment option.
External beam radiation stands as the most common treatment option for prostate cancer. Doctors use machines outside the body to direct radiation beams at the prostate. This method allows precise targeting of cancer cells while sparing healthy tissue. Most patients receive external beam radiation over several weeks. Conventional schedules involve daily sessions for six to eight weeks, with up to 40 treatments. Hypofractionated schedules deliver higher doses per session, reducing the total number of visits to as few as five weeks.
Radiation Therapy Type | Typical Duration | Session Frequency / Number of Sessions |
|---|---|---|
Conventional External Beam RT | 6 to 8 weeks | Daily treatments, total sessions up to 40 |
Hypofractionated External Beam RT | 1 to 5 weeks | Higher dose per session, fewer total sessions |
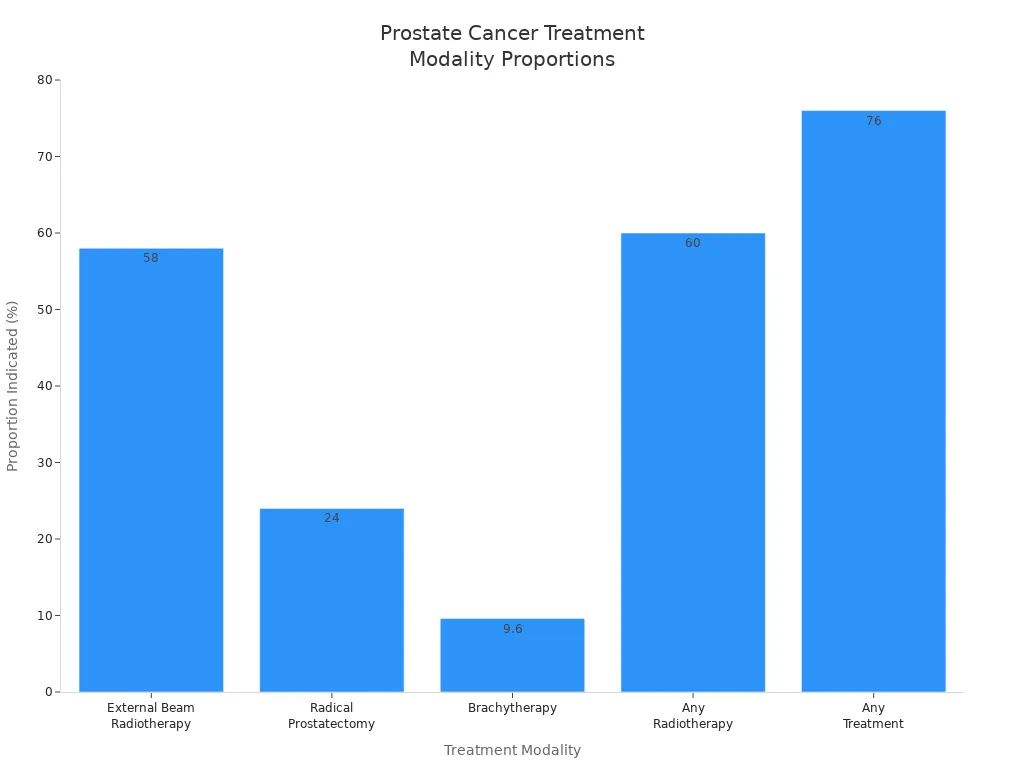
External beam radiation is indicated for 58% of prostate cancer patients, making it the leading choice compared to surgery or brachytherapy.
Treatment Modality | Proportion of Prostate Cancer Patients Indicated (%) |
|---|---|
External Beam Radiotherapy (EBRT) | 58 |
Radical Prostatectomy (RP) | 24 |
Brachytherapy (BT) | 9.6 |
Any Radiotherapy (RT) | 60 |
Any Treatment (RP, RT, or BT) | 76 |
Note: External beam radiation offers flexibility in scheduling and can be tailored to each patient’s needs.
SBRT, or stereotactic body radiation therapy, uses advanced technology to deliver high doses of radiation in fewer sessions. Doctors often recommend SBRT for prostate cancer because it shortens the overall treatment time. Most SBRT schedules involve five treatments over one to two weeks. This approach provides similar survival outcomes to conventional external beam radiation, especially when combined with hormone therapy for higher-risk patients.
Aspect | SBRT (Stereotactic Body Radiotherapy) | Conventional EBRT (External Beam Radiotherapy) |
|---|---|---|
Treatment Duration | Ultrahypofractionation: ≤5 fractions with ≥5 Gy per fraction | Smaller doses per fraction over many sessions |
Overall Survival (OS) | No significant difference compared to EBRT | Similar OS outcomes |
Cost and Convenience | More cost-effective, more convenient | Higher cost, longer duration |
Guideline Recommendations | Supported for low and intermediate risk | Standard of care across risk groups |
Evidence from Trials | HYPO-RT-PC trial supports SBRT non-inferiority | Established evidence base |
Recent clinical trials, such as NRG-GU013, compare SBRT to conventional radiation in high-risk prostate cancer. SBRT delivers five treatments over two weeks, while conventional radiation may require up to 45 sessions over nine weeks.
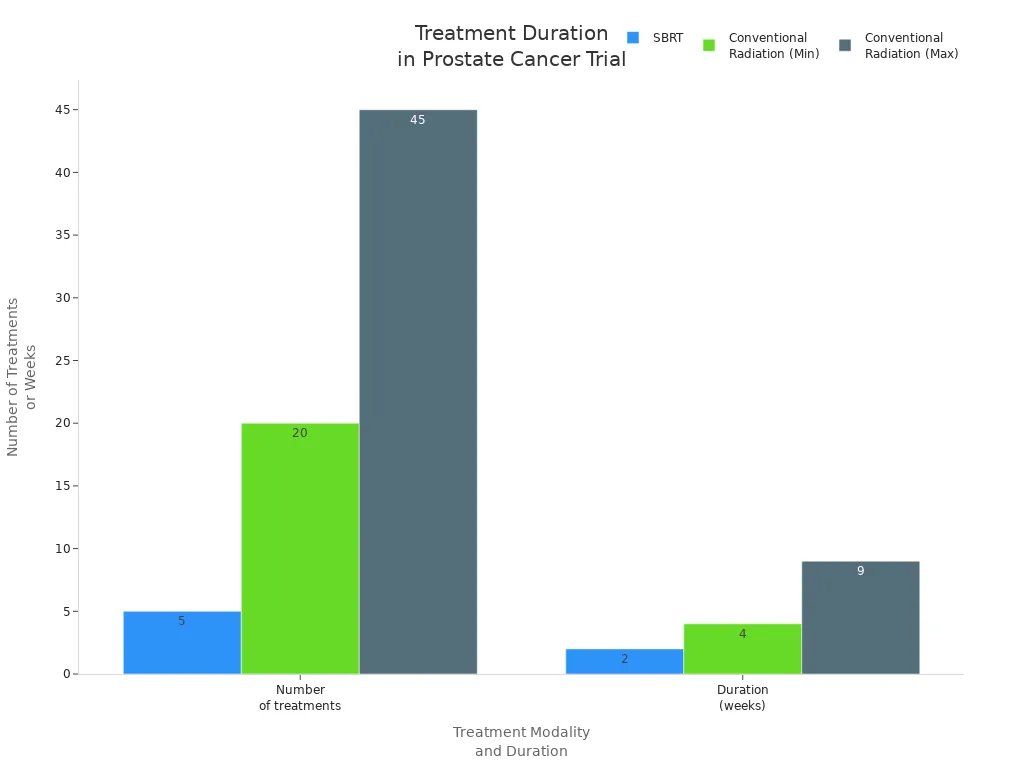
SBRT offers a shorter treatment duration with manageable side effects.
Doctors continue to study SBRT in trials for patients with prostate cancer involving pelvic lymph nodes.
SBRT provides convenience and cost savings for many patients.
Brachytherapy involves placing radioactive sources directly inside or near the prostate. Doctors use this method to deliver a concentrated dose of radiation to cancer cells. High-dose-rate (HDR) brachytherapy typically requires two sessions spaced two weeks apart. Some patients receive external beam radiation after brachytherapy, extending the total treatment time.
Treatment Type | Dose per Fraction | Number of Fractions | Interval Between Fractions | Total Approximate Duration |
|---|---|---|---|---|
HDR-Brachytherapy (HDR-BT) | 10 Gy | 2 | 2 weeks apart | 2 weeks |
EBRT after HDR-BT | 2 Gy | 25 | Daily | ~5 weeks |
Combined HDR-BT + EBRT | - | - | - | Several weeks |
EBRT only | 2 Gy | 35 | Daily | ~7 weeks |
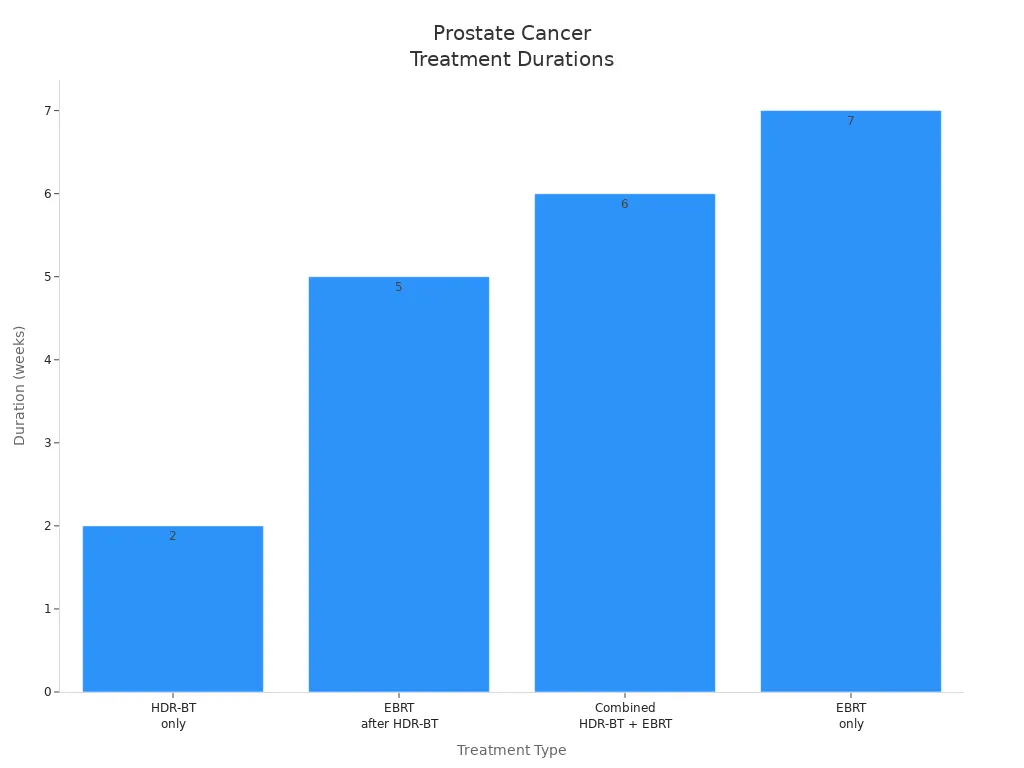
Brachytherapy suits patients with localized prostate cancer and offers a focused approach. Doctors may combine brachytherapy with external beam radiation for more advanced cases.
Tip: Patients should discuss all available radiation treatment options with their medical team to find the best fit for their prostate cancer.
Before each radiotherapy session, the medical team prepares the patient and the treatment area. The patient may need to change into a hospital gown and remove any metal objects, such as jewelry or glasses. The team reviews the treatment plan and answers any last-minute questions. They check the patient’s identification and confirm the correct treatment site. Hydration and bladder filling instructions may be given, as a full bladder can help protect healthy tissue during prostate radiotherapy. The team ensures the patient feels calm and ready before moving to the treatment room.
Precise positioning is essential for effective radiotherapy. The patient lies on a special treatment table. The team uses advanced immobilization devices to keep the patient still and comfortable. One example is the Create High Plasticity Not Shrink Fixation Radiotherapy Thermoplastic Mask. This mask softens when heated and molds closely to the patient’s features, such as the nose bridge and chin. After cooling, the mask holds its shape and keeps the patient’s head and neck in the exact position needed for treatment.
Accurate and comfortable positioning reduces movement and helps deliver radiation to the right spot every time. The thermoplastic mask system offers several advantages:
Technologists find these masks easy to use and reliable for setup.
The mask’s custom fit improves immobilization and reduces unwanted movement.
The high plasticity and non-shrink properties ensure the mask stays snug and secure.
Consistent positioning supports better treatment accuracy and patient safety.
The mask’s gentle pressure and skin-friendly material help patients feel comfortable, even during longer sessions.
Once the patient is positioned, the team leaves the room and operates the machine from a control area. The patient can communicate with the team through an intercom. The machine moves around the patient and delivers targeted radiation beams to the prostate. The process is painless, and the patient must remain still. Most sessions last between 10 and 60 minutes, depending on the treatment plan. After the session, the team removes the mask and helps the patient off the table. The patient can usually return to normal activities right away.
Reliable immobilization devices, like the Create thermoplastic mask, play a key role in making each session safe, accurate, and as comfortable as possible.

Prostate cancer patients often adjust their routines during radiotherapy. Many continue working, though energy levels may change. Some work full-time, while others switch to part-time or take breaks, depending on fatigue. Fatigue usually increases as therapy progresses and can last for weeks or months after treatment ends. Exercise helps improve sleep and manage side effects. Even light activities, such as walking or stretching, benefit overall well-being. Patients do not become radioactive from external radiation therapy, so they safely spend time with family and friends. Emotional challenges, including anxiety and fear, may arise. Support groups, relaxation techniques, and counseling help patients cope.
Ability to work varies for each patient.
Fatigue tends to increase during therapy.
Exercise supports recovery and well-being.
Patients remain safe for close contact with loved ones.
Emotional support is important for mental health.
Prostate cancer patients report side effects that affect daily life, such as urination problems, bowel issues, and disturbed sleep. Despite these challenges, most describe the treatment period positively. They experience uncertainty at first, but support from partners and healthcare professionals helps them develop new routines and cope with side effects.
Radiotherapy for prostate cancer causes several common side effects. These effects may appear during therapy or months after treatment ends. The table below summarizes the most frequent side effects and their timing:
Side Effect Category | Specific Side Effects | Frequency / Timing |
|---|---|---|
Urinary | Urgency, frequency, burning, incontinence | Early symptoms common; about 50% experience leakage years later |
Bowel | Looser stools, irritation, diarrhea, rectal bleeding | Common early and delayed; early issues may predict long-term problems |
Sexual Function | Erectile dysfunction, reduced libido, changes in ejaculation | Common delayed effect; many retain function initially |
Fatigue | Feeling very tired | Most common during and after treatment; can last months |
Skin | Redness, dryness, irritation | Common during therapy; managed with gentle care |
Rare but Severe | Chronic cystitis, pelvic fibrosis, secondary cancers | Rare; may develop months to years after therapy |
Fatigue stands out as the most common side effect. Urinary and bowel symptoms often appear early and may persist. Sexual function changes usually develop over time. Skin irritation occurs in the treated area but responds well to gentle care.
Patients receive support from many sources during radiotherapy. Education materials help them understand their treatment and prepare for each visit. Support and information services guide patients through therapy. Community resources offer group support and connection with others facing similar challenges. Financial assistance programs help manage costs related to treatment. Preparation guides reduce anxiety and improve readiness for therapy sessions.
Patient education materials explain the treatment process.
Support services provide information and guidance.
Community resources connect patients with local groups.
Financial assistance programs ease the burden of treatment costs.
Preparation guides help patients feel ready for therapy.
These resources help patients feel informed and supported throughout their therapy journey. Access to support improves confidence and helps patients manage the challenges of prostate cancer treatment.
Doctors sometimes adjust radiotherapy schedules for prostate cancer. These changes can happen for many reasons. A patient might feel unwell on a treatment day. The clinic could need to reschedule because of equipment checks or holidays. Sometimes, side effects become too strong, and the doctor decides to pause treatment for a short time.
Patients should know that small changes in the schedule usually do not affect the success of treatment. The medical team tracks each session and makes sure the patient receives the full planned dose. If a patient misses a session, the team often adds an extra day at the end of the schedule.
Tip: Patients should tell the clinic as soon as possible if they cannot attend a session. Early notice helps the team plan and keep treatment on track.
Here are some common reasons for schedule changes:
Illness or fever
Severe side effects, such as skin irritation or fatigue
Family emergencies
Public holidays or clinic closures
Equipment maintenance
Doctors always aim to keep the treatment as close to the original plan as possible. They know that regular sessions help the radiation work best. When changes happen, the team explains the new plan and answers questions.
Clear communication between patients and the medical team supports successful radiotherapy. Patients should share any new symptoms or concerns right away. The team can help manage side effects and adjust care if needed.
Doctors and nurses encourage patients to ask questions about their treatment. They explain each step and provide written information. Many clinics offer a contact number for urgent questions. Some patients keep a notebook to track symptoms and questions for their next visit.
Note: Good communication helps patients feel more confident and less anxious during treatment.
Ways patients can improve communication:
Write down questions before appointments
Bring a family member or friend for support
Use a notebook to record symptoms and side effects
Ask for written instructions or educational materials
Contact the clinic if problems arise between sessions
The medical team wants every patient to feel informed and supported. Open conversations help the team deliver safe, effective care. Patients who speak up about their needs often have a better experience during radiotherapy.
Radiotherapy for prostate cancer offers several schedules, ranging from short courses to longer treatments. Each session uses precise positioning and modern techniques to improve comfort and accuracy. Patients receive support from medical teams and have options for adjusting their plans.
Treatment duration varies based on individual needs.
Support and flexibility help patients manage therapy.
Open communication with healthcare providers ensures the best care and answers to personal questions.
Most sessions take 10 to 60 minutes. The exact time depends on the treatment type and the need for precise positioning. The medical team works to keep each session as short and comfortable as possible.
Many patients continue working during treatment. Some adjust their schedules or take breaks if they feel tired. Doctors encourage patients to listen to their bodies and rest when needed.
External beam radiotherapy does not make patients radioactive. They can safely spend time with family and friends after each session. Only some forms of brachytherapy require special precautions.
Technologists use immobilization devices, such as the Create High Plasticity Not Shrink Fixation Radiotherapy Thermoplastic Mask. These devices keep patients still and comfortable, improving treatment accuracy.
Most side effects improve over time. Some, like fatigue or skin irritation, fade within weeks. Others, such as urinary or bowel changes, may last longer. Doctors monitor patients and offer support for any lasting symptoms.
Patients should contact the clinic as soon as possible. The medical team reschedules missed sessions and ensures the full treatment plan continues. Small changes in schedule rarely affect treatment success.
Most patients spend about 30 to 60 minutes on a CT simulation, with some sessions taking up to 90 minutes for complex cases. The process remains straightforward and centers on patient comfort. CT simulation serves as a crucial step before radiation therapy. Staff use advanced equipment and clear instructions to help patients feel at ease throughout the session.
Thermoplastic splints have become increasingly popular in the medical field due to their versatility and effectiveness in treating a wide range of conditions. In this article, we will explore the various uses and benefits of thermoplastic splints, shedding light on how they can aid in the recovery p
IntroductionRadiotherapy is a crucial treatment for many types of cancer, utilizing high-energy radiation to target and destroy cancer cells. During treatment, precision is key to ensuring that the radiation is directed at the tumor while minimizing exposure to surrounding healthy tissues. This is w
Have you ever wondered how doctors plan precise cancer treatments? CT simulation plays a critical role in radiation therapy by creating detailed 3D images of the body. This advanced technology ensures that radiation is delivered accurately to target tumors, minimizing damage to surrounding healthy tissue.
CT Simulation is a crucial step in radiation therapy. It ensures accurate treatment by mapping the precise location of cancer cells. Without proper preparation, the accuracy of radiation delivery can be compromised, which could affect the treatment's effectiveness.