
Radiotherapy uses high-energy radiation to target and destroy cancer cells while protecting healthy tissue.
Advanced imaging and technology help doctors deliver precise radiation doses, improving treatment success and reducing side effects.
There are three main types of radiotherapy: external beam, internal (brachytherapy), and systemic treatment, each suited for different cancers.
Radiotherapy can aim to cure cancer, control its growth, or relieve symptoms to improve quality of life.
Success rates of radiotherapy are high, especially in early-stage cancers, and combining it with other treatments can boost outcomes.
Side effects are common but usually manageable; your care team will help you reduce and cope with them during and after treatment.
Radiotherapy is safe for most patients, with new techniques lowering risks and supporting daily activities during treatment.

Radiation therapy is a medical procedure that uses high-energy radiation to treat cancer. You may receive this treatment as part of your overall cancer care. Doctors use radiation therapy to target tumors and destroy cancer cells while sparing as much healthy tissue as possible. This approach forms a key part of many radiotherapy treatment plans.
You will find that radiation therapy can be delivered externally or internally, depending on the type and location of your tumor. The goal is to deliver a high dose of radiation directly to the tumor, which helps shrink or eliminate it. Your doctor will use advanced imaging techniques to map out the exact position of your tumor before starting the radiation therapy procedure. This ensures that the treatment plan is as precise as possible.
Note: Imaging plays a crucial role in every step of radiation therapy. It helps your care team visualize the tumor, plan the treatment, and monitor your progress.
Radiation therapy works by damaging the DNA inside cancer cells. This damage prevents the cells from dividing and growing, which leads to their destruction. The process relies on both direct and indirect effects of radiation on the tumor.
When you undergo radiation treatment, the main goal is to destroy cancer cells while protecting healthy tissue. Here is how radiation therapy targets cancer at the cellular level:
Radiation causes DNA damage in cancer cells, including single-strand breaks and double-strand breaks. Double-strand breaks are the most lethal.
The energy from radiation can act directly on the DNA or indirectly by creating free radicals from water molecules inside the cell.
Damaged DNA blocks the cancer cell’s ability to divide and proliferate, leading to cell death.
Cancer cells often have weaker DNA repair mechanisms than healthy cells, making them more vulnerable to radiation.
The p53 protein helps control how cells respond to DNA damage. It can trigger cell cycle arrest, apoptosis (programmed cell death), or senescence (permanent loss of the ability to divide).
Radiation can activate complex signaling pathways that influence how sensitive or resistant a tumor is to treatment.
Inhibiting certain DNA repair proteins can make cancer cells even more sensitive to radiation.
Types of cell death caused by radiation include apoptosis, mitotic catastrophe, necrosis, senescence, and autophagy.
Radiation therapy aims to minimize harm to healthy tissue, but some effects on normal cells can occur. Here is what happens:
Healthy cells can also experience DNA damage from radiation, but they usually repair this damage more efficiently than cancer cells.
Advanced imaging and precise targeting help reduce the exposure of healthy tissue to high doses of radiation.
Radiation can affect cell membrane signaling pathways, which may influence how both cancer and healthy cells respond to treatment.
The immune system can recognize and attack cancer cells more effectively after radiation alters the tumor’s immunogenicity.
The bystander effect allows irradiated tumor cells to send signals that can kill nearby cancer cells, often sparing normal tissue.
Your care team uses imaging throughout the radiotherapy process to monitor the tumor and adjust the treatment plan as needed.
Recent advancements in radiotherapy technology have improved patient outcomes. Proton therapy, for example, delivers radiation with pinpoint accuracy, reducing damage to healthy tissues. Pencil beam scanning and adaptive radiotherapy use real-time imaging to shape the radiation dose to the unique contours of your tumor. These innovations allow you to complete more treatment cycles with fewer side effects and better results.
Tip: Ask your care team about the imaging techniques and technologies used in your radiotherapy treatment plan. Understanding these tools can help you feel more confident and informed about your care.
Radiotherapy includes several main approaches. You may receive external radiotherapy, internal radiotherapy (brachytherapy), or systemic treatment. Each method uses radiation in a unique way to target cancer and support your treatment plan.
External radiotherapy, also called teletherapy, delivers radiation from a machine outside your body. You will lie on a treatment table while the machine aims radiation beams at your tumor. Teletherapy uses advanced imaging to plan and guide each session, making sure the radiation targets the cancer precisely.
You may encounter several types of external radiation therapy in clinical practice:
External beam therapy remains the most common form of teletherapy.
AlignRT tracks your movement to keep you in the correct position.
CT-guided imaging shapes the radiation beams to match your tumor.
Image-guided radiation therapy (IGRT) uses repeated imaging during sessions for accuracy.
Intensity-modulated radiation therapy (IMRT) adjusts beam strength for better tumor targeting.
Stereotactic radiosurgery (SRS) treats brain tumors with high precision.
Stereotactic body radiotherapy (SBRT) targets tumors in areas like the neck, spine, or lung.
Total Body Irradiation (TBI) prepares you for stem cell transplantation.
Proton therapy uses protons to treat tumors near sensitive tissues.
Description | How It Works | Typical Treatment Schedule | |
|---|---|---|---|
3-D Conformal Radiation Therapy | Uses CT, MRI, PET images to plan and shape radiation beams to tumor shape | Delivers beams from many directions to conform to tumor, sparing normal tissue | Usually once a day, Monday to Friday; number of treatments varies by cancer specifics |
Intensity-Modulated Radiation Therapy (IMRT) | Advanced form of 3-D conformal therapy with many smaller beams of varying strength | Targets tumor with modulated beam intensities for higher dose to tumor and sparing normal tissue | Usually once a day, Monday to Friday; varies by patient |
Image-Guided Radiation Therapy (IGRT) | Type of IMRT using imaging scans during treatment sessions | Repeated scans during treatment adjust beam position/dose for accuracy | Usually once a day, Monday to Friday; varies by patient |
Stereotactic Radiosurgery (SRS) | Focused high-energy beams for small brain tumors | Multiple small beams converge on tumor; patient immobilized during treatment | Usually single dose or up to five doses once per day |
Stereotactic Body Radiation Therapy (SBRT) | Similar to SRS but for body tumors | Delivers high doses precisely to body tumors | Fewer sessions than standard radiation |
Proton Therapy | Uses protons instead of photons for localized tumors near sensitive tissue | Protons release energy at specific depth, sparing normal tissue | Treatment schedule varies |
Teletherapy often requires daily visits over several weeks. You will not feel the radiation during the session. Imaging ensures the radiation treatment remains accurate and safe.
Internal radiotherapy, also known as brachytherapy, places radioactive material inside or next to your tumor. This method delivers a high dose of radiation directly to the cancer, reducing exposure to healthy tissues. You may receive brachytherapy for cancers such as prostate, cervix, uterus, or breast.
You will follow several steps during brachytherapy:
Meet with your radiation oncologist for imaging scans and treatment planning.
Prepare for the procedure, which may include medication or fasting.
Enter a special brachytherapy suite with imaging and anesthesia equipment.
The care team places radioactive sources inside your body using tubes, needles, or applicators.
Receive radiation treatment, which may last minutes (high-dose rate) or days (low-dose rate).
Recover in a monitored area and receive instructions for aftercare and safety.
Precise positioning is essential for successful brachytherapy. Your care team uses advanced immobilization devices to keep you comfortable and still during the procedure. The Create Immobilization Premium Brachytherapy Transfer Board supports you with air flotation technology, making transfers smooth and comfortable. Carbon fiber construction keeps the board strong yet lightweight. The electric lift and remote control allow easy adjustments, while the brake function ensures stability. Adjustable leg supports and compatibility with thermoplastic masks or vacuum fixation mats help your team achieve the best positioning for your treatment. These features improve both comfort and accuracy, supporting the effectiveness of your internal radiotherapy.
Systemic radiation therapy uses radioactive drugs that travel through your bloodstream to reach cancer cells throughout your body. You may receive this type of radiation treatment for cancers such as prostate, thyroid, lymphoma, bone, breast, lung, leukemia, multiple myeloma, and neuroendocrine tumors. Systemic treatment allows your care team to target cancer that has spread beyond the original site. Imaging helps monitor how the radioactive drug moves and where it collects in your body, guiding your treatment plan.
If you have questions about which type of radiotherapy is right for you, ask your care team. They will use imaging and other tests to recommend the best approach for your cancer.
When you start cancer treatment, your care team sets clear goals based on your unique situation. The main goal often focuses on curing cancer or controlling its growth. You may hear your doctor talk about achieving permanent control of the tumor and any spread to nearby lymph nodes. Your team works to destroy as many cancer cells as possible while protecting healthy tissue.
Several factors help your doctor decide on the best approach:
The type and grade of your tumor
The stage of the cancer
Your overall health and performance status
Biological features of the tumor, such as how fast it grows or repairs DNA
Doctors now use advanced imaging and molecular data to personalize your treatment. These tools help your team track how your tumor responds and adjust your plan if needed. Predictive biomarkers can guide the dose and schedule of radiotherapy, making your care more precise. The goal is always to give you the best chance to cure cancer or keep it under control.
Your treatment plan is unique to you. Your care team considers every detail to help you reach the best possible outcome.
Sometimes, the main goal of radiotherapy is not to cure the disease but to relieve symptoms and improve your quality of life. This approach is called palliative radiotherapy. You may receive this type of treatment if your cancer has spread or if a cure is not possible.
Palliative radiotherapy helps you manage symptoms such as:
Pain from bone tumors or metastases
Bleeding from tumors in the lungs, digestive tract, or other organs
Obstructions that make it hard to breathe or eat
Neurological problems caused by tumors in the brain or spine
You usually receive palliative radiotherapy in a short course, often between 1 and 10 sessions. The doses are lower than those used to cure cancer, which helps reduce side effects and makes the process easier for you. The main goal is to relieve symptoms quickly and help you feel better.
Many cancer patients find that palliative radiotherapy brings fast relief and allows them to enjoy daily activities again.
Your doctor decides when to use radiotherapy by looking at several clinical criteria. The stage and pathology of your tumor play a big role. For example, your care team may check PSA levels or Gleason scores for prostate cancer. They also consider your anatomy, past surgeries, and other health conditions.
Imaging and careful planning help your team target the tumor accurately. Techniques like daily CT scans or using markers inside your body make sure the radiation hits the right spot. Your doctor may choose different methods, such as intensity-modulated radiation therapy or proton therapy, based on what works best for your body and tumor location.
A group of experts reviews the latest research and creates guidelines to help doctors decide when radiotherapy is right for you. These guidelines ensure that every patient receives care tailored to their specific needs.
If you have questions about your treatment options, ask your care team. They will explain why radiotherapy may help you and how it fits into your overall cancer treatment plan.
You may wonder how effective radiation therapy is for different types of cancer. The success of this treatment depends on many factors, but data shows that radiation can achieve high control rates, especially in early-stage cancer. For example, if you receive radiation for Stage I cancer, you have a reported success rate between 90% and 95%. As the stage advances, the success rate decreases, but radiation still offers strong results.
Cancer Stage | Reported Success Rate of Radiotherapy |
|---|---|
Stage I | 90-95% |
Stage II | 85-90% |
Stage III | 75-80% |
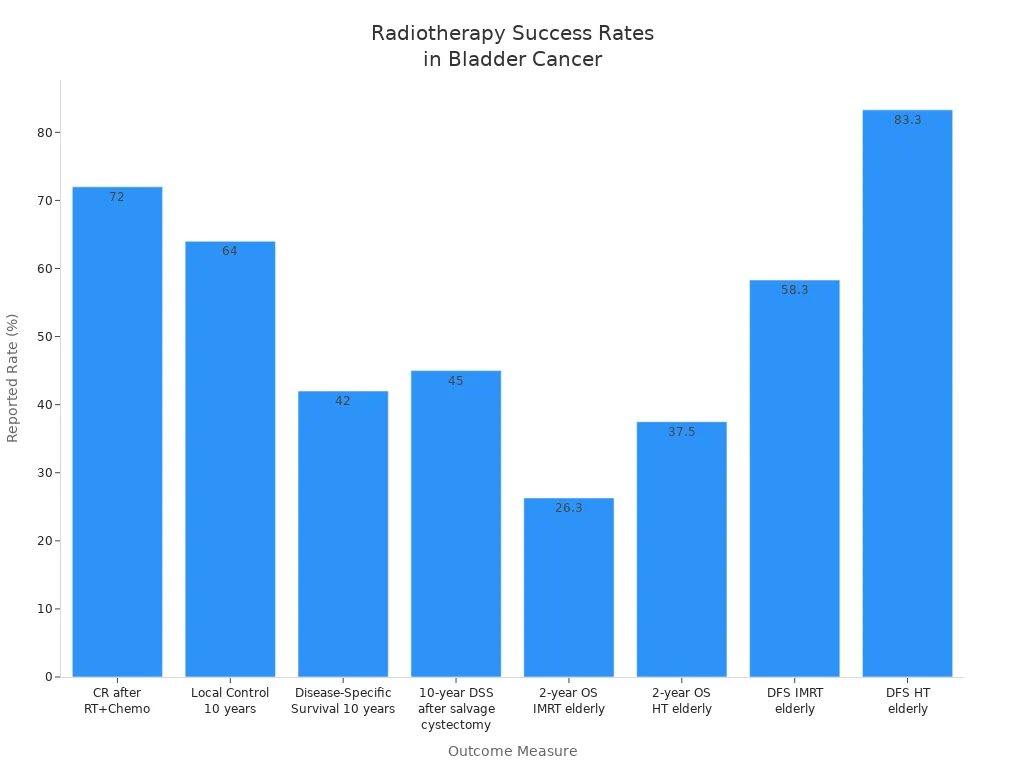
Radiation therapy also works well when combined with other treatments, such as chemotherapy. In bladder cancer, combining radiation and chemotherapy leads to a complete response in about 72% of patients. Long-term control and survival rates remain promising, even after ten years.
Outcome Measure | Reported Rate/Statistic |
|---|---|
Complete Response (CR) after RT+Chemo | 72% |
Local Control at 10 years | 64% |
Disease-Specific Survival at 10 years | 42% |
10-year Disease-Specific Survival after salvage cystectomy | 45% |
2-year Overall Survival (IMRT, elderly) | 26.3% |
2-year Overall Survival (HT, elderly) | 37.5% |
Disease-Free Survival (IMRT, elderly) | 58.3% |
Disease-Free Survival (HT, elderly) | 83.3% |
Some cancers respond even better to special radiation schedules. For example:
Hyperfractionation in head and neck cancer improves 5-year local control by 49% and survival by 33%.
Continuous hyperfractionated accelerated radiation in lung cancer increases 2-year survival by 43%.
Squamous carcinoma patients see a 65% increase in 2-year survival with these advanced schedules.
These results show that radiation therapy can play a powerful role in your cancer treatment plan.
Your outcome with radiation therapy depends on more than just the type of cancer. Several patient factors can influence how well you respond to treatment. You should consider the following:
Patient Factor | Influence on Radiotherapy Outcomes |
|---|---|
Younger patients usually tolerate radiation better. Older patients may have reduced tissue repair. Gender differences can affect mortality and may require different approaches. | |
Comorbidities & Health | Conditions like heart disease or diabetes can lower your ability to handle radiation side effects. Your care team will check your overall health before starting treatment. |
Genetic Factors | Your DNA repair ability affects how sensitive you are to radiation. Some people recover faster, which helps personalize your therapy. |
Immune System | A strong immune response can make radiation more effective. Combining radiation with immune therapies may improve your results. |
Other important factors include:
How well you can care for yourself during treatment
The type and stage of your disease
Your attitude and your family's support for your treatment plan
Your care team will look at all these factors to design the safest and most effective radiation therapy for you. Staying positive and involved in your care can help you achieve the best possible outcome.

Radiation therapy can help you fight cancer, but it may also cause side effects. These effects depend on the area treated, the dose, and your overall health. Most people experience some short-term side effects during or soon after radiotherapy. Some may also notice long-term changes months or years later.
You may notice short-term side effects soon after starting radiation. These usually improve within weeks after treatment ends. The most frequently reported short-term side effects include:
Fatigue: You may feel tired or low on energy, even after rest.
Skin irritation: The treated area can become red, dry, itchy, or peel. This is called radiation dermatitis.
Nausea and vomiting: These symptoms often occur if you receive radiation to your abdomen or digestive tract.
Diarrhea: Pelvic or abdominal radiation can irritate your bowels.
Acute cardiovascular effects: Some people develop heart inflammation, such as pericarditis, shortly after treatment.
Hair loss and mouth problems: These occur only in the area treated.
Most early side effects are mild and treatable. Your care team will help you manage them so you can complete your therapy.
Some side effects may appear months or years after radiation therapy. These long-term effects depend on the area treated and your individual risk of side effects. The table below shows how often certain long-term side effects occur in different cancer types:
Cancer Type | Long-term Side Effect | Percentage of Patients |
|---|---|---|
Head and Neck | Swallowing difficulties at 6 years | 71% |
Head and Neck | Aspiration | 20% |
Head and Neck | Required laryngectomy | 7% |
Prostate (with early acute toxicity) | Late urinary toxicity increase | |
Prostate (with early acute toxicity) | Late bowel toxicity increase | 12.7% to 22.5% |
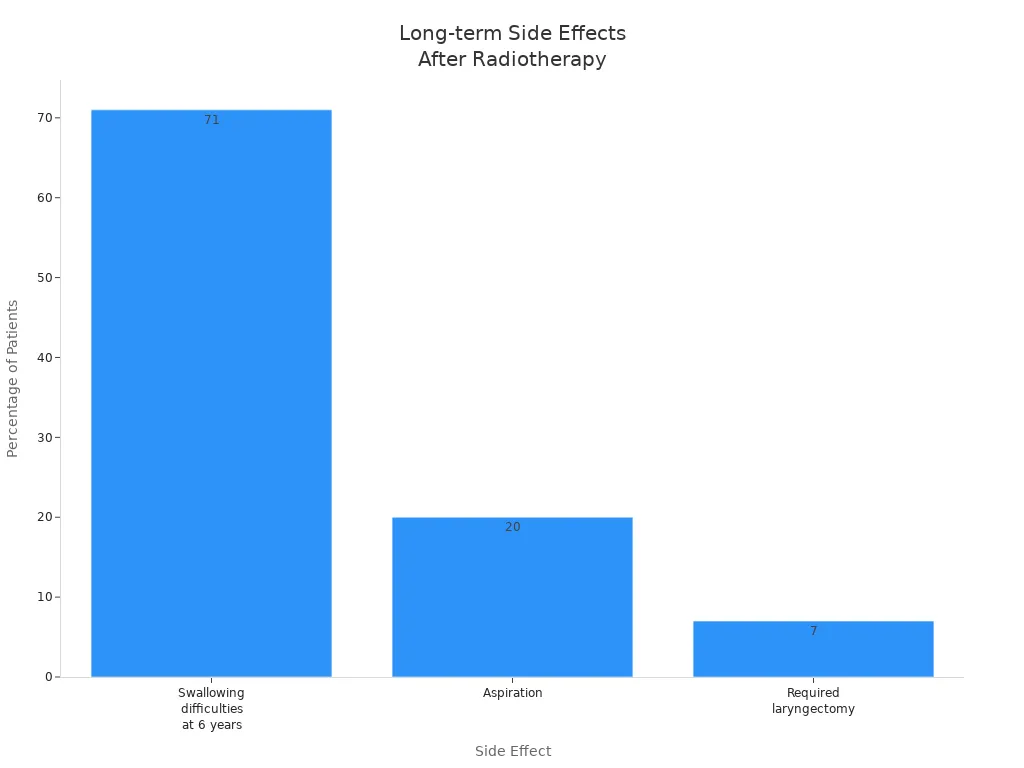
You should talk to your care team about your personal risk of side effects and how to monitor for late changes.
You can take steps to reduce and manage side effects during and after radiation therapy. Your care team will guide you, but here are some proven strategies:
Practice good skin care: Protect treated skin from sun, heat, and cold. Wear loose clothing and avoid harsh products.
Manage fatigue: Rest when needed and conserve your energy. Gentle exercise can help reduce tiredness.
Address mouth and throat changes: Acupuncture may help dry mouth. Honey and special licorice can soothe mouth sores.
Control diarrhea: Probiotics and, in some cases, glutamine may help balance your gut.
Eat well: Small, frequent meals and plenty of fluids support your recovery. Nutritional counseling can improve your quality of life.
Care for hair and scalp: Use mild shampoo and protect your scalp from sun and cold if you lose hair in the treated area.
Communicate: Tell your care team about any symptoms. They can adjust your plan and offer support.
Managing side effects is a team effort. Stay in touch with your care team and ask for help when you need it.
Radiation therapy is a well-studied and effective cancer treatment. Most people complete radiotherapy safely, but all treatments carry some risk of side effects. Newer techniques, such as proton therapy, can lower the risk of severe side effects and help you maintain your daily activities. For example, studies show that only 12% of patients receiving proton therapy needed hospitalization for severe side effects within 90 days, compared to 28% with traditional radiation. Cancer control and survival rates remain similar between these methods.
Advanced technology now helps predict your personal risk of side effects before treatment begins. AI models can analyze your medical data and improve safety by anticipating possible reactions. These tools help your care team tailor your plan and reduce unwanted effects.
You can feel confident that radiation therapy is safe for most patients. Your care team will use the latest tools and knowledge to protect your health while treating your cancer.
You will meet with your doctor before starting your course of treatment. The team will gather important information to create a plan that fits your needs. You can expect several assessments:
Your doctor will take a thorough medical history and perform a physical examination, including checking your neck and cranial nerves.
The team will review diagnostic tests such as MRI, CT, X-ray images, pathology reports, and lab results.
A speech-language pathologist may evaluate your speech and swallowing to see how well you can tolerate treatment.
A dietitian will assess your nutrition to make sure you have enough calories before, during, and after your course of treatment.
Dental clearance is important. Your doctor will check your oral health and may recommend fluoride treatments.
Medical clearance from your primary care physician and other specialists confirms you are fit for treatment and anesthesia.
If you have severe symptoms, urgent interventions like a tracheostomy or feeding tube may be considered.
Your doctor will explain each step and answer your questions. You should feel comfortable sharing any concerns about your upcoming treatment.
You will attend daily treatment sessions as part of your course of treatment. Most patients receive outpatient care, so you can continue your regular activities. Here is what you can expect during each session:
The team will position you and set up equipment, which usually takes 5 to 15 minutes.
Immobilization devices help keep you in the same position every day for accuracy.
After positioning, the radiation therapist leaves the room but monitors you remotely and communicates through a microphone.
The treatment machine may make clicking or whirring noises. These sounds are normal.
The radiation beam targets your tumor, minimizing exposure to healthy tissue.
Sessions are painless and feel similar to getting an X-ray.
Treatments are scheduled five days a week, typically lasting 3 to 10 weeks, depending on your cancer type and plan.
The time between daily treatments allows healthy cells to repair.
Your doctor and therapy team monitor your progress and adjust your plan as needed.
Tip: You can ask your doctor about the schedule and what to expect during each session. Staying informed helps you feel more confident.
After your treatment ends, you need to care for your skin and monitor your health. Proper aftercare reduces side effects and supports recovery. Follow these recommendations:
Bathe or shower daily with warm water and mild, unscented soap. Avoid scrubbing treated skin.
Moisturize treated areas twice a day with fragrance-free, lanolin-free products. Do not apply to broken skin.
Wear loose-fitting cotton clothing to reduce irritation.
Avoid makeup, perfumes, powders, deodorants, and sticky adhesives on treated skin.
Protect your skin from extreme temperatures. Do not use hot tubs, heating pads, or ice packs.
If you need to shave, use an electric razor and stop if irritation occurs.
Use PABA-free sunscreen with SPF 30 or higher, wear sun-protective clothing, and seek shade.
Avoid tanning beds and burning your skin for life.
Monitor your skin for changes like redness, rash, blisters, or itching. Report these to your doctor promptly.
Schedule regular dermatology appointments for ongoing skin evaluation.
Note: Skin reactions may peak up to two weeks after treatment ends. Some side effects can appear months or years later. Your doctor will guide you through recovery and answer any questions.
You often receive radiotherapy as part of a larger treatment plan. Doctors combine it with surgery or chemotherapy to improve your chances of beating cancer. Clinical studies show that among patients who survive at least five years, 80% have surgery, 39% receive radiotherapy, and 29% get chemotherapy. Nearly half of these patients benefit from two treatments together, and 13% receive all three. This approach, called multi-modality treatment, uses the strengths of each therapy. You may have surgery to remove a tumor, followed by radiotherapy to destroy any remaining cancer cells. Chemotherapy can work with radiotherapy to target cancer throughout your body. Your care team will design a plan that fits your specific needs and the type of cancer you have.
Researchers also study how radiotherapy works with immunotherapy. When you combine radiotherapy with immune checkpoint inhibitors, you may see better results. Studies in melanoma, breast cancer, and lung cancer show improved survival and lower recurrence rates. For example:
Adding anti-PD-1 antibodies to stereotactic radiation therapy increases survival in brain tumor models.
Patients with non-small cell lung cancer who receive radiotherapy before pembrolizumab live longer.
Combining stereotactic radiosurgery with checkpoint inhibitors boosts 12-month survival rates.
This combination helps your immune system recognize and attack cancer cells more effectively.
Your doctor will consider these options to give you the best possible outcome.
Radiotherapy plays a key role in treating many cancers. You may receive it as a primary treatment or as an extra step after surgery. For early-stage breast cancer, radiotherapy after breast-conserving surgery lowers the risk of the cancer coming back. In head and neck cancers, doctors use radiotherapy to improve control when surgery cannot remove all the tumor or when the tumor is close to important structures. Central nervous system tumors also respond well to radiotherapy, especially when surgery leaves behind some cancer cells.
Doctors recommend radiotherapy after surgery for orofacial cancers if the tumor is large or has spread to lymph nodes. In advanced laryngeal carcinoma, you may need radiotherapy to control small amounts of cancer left after surgery. Melanoma patients benefit from radiotherapy after lymph node dissection, especially when the disease is bulky or hard to remove completely. This treatment helps control cancer locally and can provide modest survival benefits. Your care team will choose radiotherapy based on the type of cancer and your unique situation.
You do not have to face radiotherapy alone. Many support resources help you and your loved ones during treatment. You can access educational materials like pamphlets, videos, and facility tours to learn what to expect. Nurses may offer sexual rehabilitation programs that include your partner, helping you manage relationship changes. Psychological support, such as art therapy or imaginative stabilization techniques, can ease anxiety and improve your well-being.
Continuous care from your healthcare team makes a big difference. When you receive clear, trustworthy information about side effects and aftercare, you feel more prepared and less anxious.
Couple-based interventions help both you and your caregiver manage stress and emotions. Studies show that patients want information tailored to their needs and delivered at the right time. When you get the support you need, you feel more confident and satisfied with your care. Remember, your care team is there to guide you every step of the way.
You gain powerful options with radiotherapy, which uses high-energy radiation therapy to target and destroy cancer cells while sparing healthy tissue. Your doctor works with a multidisciplinary team to tailor each treatment plan, using advanced imaging and patient feedback to improve safety and results. Side effects vary, but your care team helps you manage them. For further support, explore resources from the Radiological Society of North America and the European Society for Radiotherapy and Oncology. Always consult your doctor for advice that fits your unique needs.
Radiological Society of North America (RSNA): Comprehensive patient education and support
European Society for Radiotherapy and Oncology (ESTRO): Research articles and clinical guidance
You do not feel pain from the radiation itself. The machine may make noises, but you stay comfortable. Most sessions last only a few minutes. Your care team monitors you throughout each session.
You can usually maintain your routine. Most patients work, exercise, and spend time with family. Fatigue may affect your energy, so plan rest periods. Your doctor will advise you based on your treatment plan.
Doctors use special techniques to protect children and older adults. Your care team adjusts doses and uses advanced imaging to minimize risks. Safety remains a top priority for every patient.
You meet with your doctor for planning. You may need imaging scans and blood tests. Wear comfortable clothing. Follow instructions about eating, drinking, or taking medications before your appointment.
Eat small, frequent meals with protein, fruits, and vegetables. Drink plenty of water. Avoid spicy or acidic foods if you have mouth or throat irritation. A dietitian can help you choose the best options.
Hair loss only occurs in the area treated. If you receive radiation to your head, you may lose scalp hair. Radiation to other body parts does not affect hair elsewhere.
Tip: Use fragrance-free moisturizer twice daily. Wear loose cotton clothing. Protect your skin from sun and extreme temperatures. Report any redness, rash, or blisters to your doctor promptly.
Some patients experience long-term effects months or years later. Your risk depends on the area treated and your health. Regular follow-up visits help your care team monitor and manage any changes.
Most patients spend about 30 to 60 minutes on a CT simulation, with some sessions taking up to 90 minutes for complex cases. The process remains straightforward and centers on patient comfort. CT simulation serves as a crucial step before radiation therapy. Staff use advanced equipment and clear instructions to help patients feel at ease throughout the session.
Thermoplastic splints have become increasingly popular in the medical field due to their versatility and effectiveness in treating a wide range of conditions. In this article, we will explore the various uses and benefits of thermoplastic splints, shedding light on how they can aid in the recovery p
IntroductionRadiotherapy is a crucial treatment for many types of cancer, utilizing high-energy radiation to target and destroy cancer cells. During treatment, precision is key to ensuring that the radiation is directed at the tumor while minimizing exposure to surrounding healthy tissues. This is w
Have you ever wondered how doctors plan precise cancer treatments? CT simulation plays a critical role in radiation therapy by creating detailed 3D images of the body. This advanced technology ensures that radiation is delivered accurately to target tumors, minimizing damage to surrounding healthy tissue.
CT Simulation is a crucial step in radiation therapy. It ensures accurate treatment by mapping the precise location of cancer cells. Without proper preparation, the accuracy of radiation delivery can be compromised, which could affect the treatment's effectiveness.